Cervical cancer, once a leading cause of death for women, has seen a significant reduction in the past four decades due to the widespread use of routine Pap tests and human papillomavirus (HPV) testing. Despite progress, around one-third of cases arise in women with normal Pap results,¹ underscoring the importance of continuous vigilant screening. Annually, 13,960 people are diagnosed with cervical cancer in the U.S., resulting in 4,310 deaths.²
While Pap cytology has been in use since 1928,³ recent technological advances in HPV testing have provided clinicians with the ability to identify patients at higher risk of cervical cancer based on their HPV genotype.
More than nine out of every 10 cases of cervical cancer are caused by HPV.⁴ While more than 80% of women and men acquire HPV by age 45, HPV infection has no age limit.⁵ Diagnostic testing remains crucial, especially since not every HPV-exposed woman returns for subsequent testing. Recognizing this challenge, Roche Diagnostics, committed to shaping a future with longer, healthier lives, offers a comprehensive FDA-approved Cervical Cancer Portfolio. Our innovative solutions aim to address screening limitations, enabling earlier diagnosis and treatment that prioritize patient well-being.
Advances in cervical cancer screening and triage
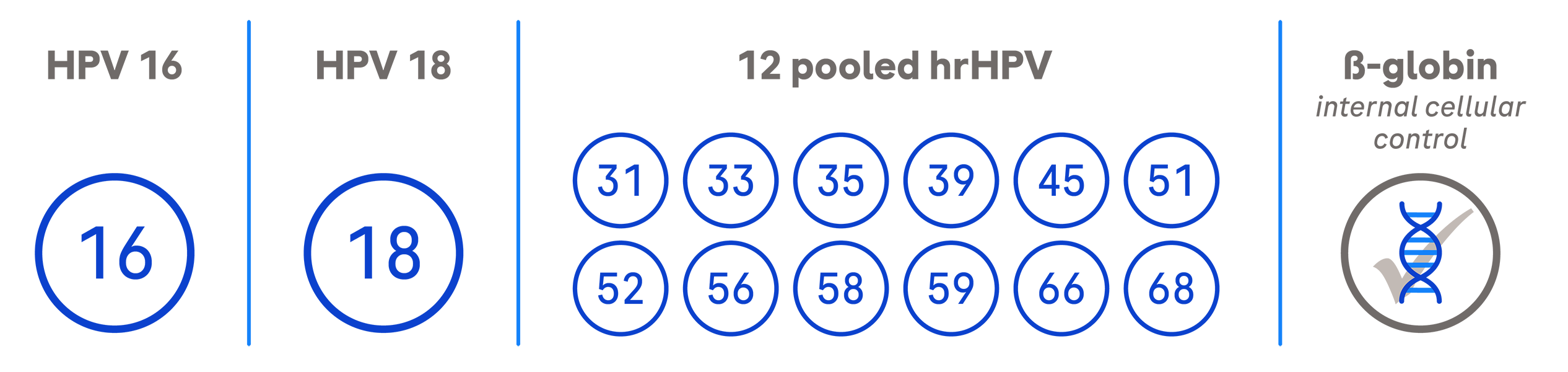
Our test can detect high-risk HPV genotypes, including HPV-16 and HPV-18 and 12 other pooled genotypes.
A more recent innovation, the dual-stain triage technology, can detect the transformation of HPV-infected cells into precancer. For example, in a dual-stain biomarker triage test, p16 is a biomarker that occurs in normal cells and signifies cell cycle arrest. Ki-67 is also a biomarker that occurs in normal cells and signifies cell cycle division. A new test can identify when both biomarkers are present at the same time, indicating that HPV is disrupting the cell cycle and the cell has started to transform.
Early detection significantly improves the five-year survival rate, which is 92% for women with invasive cervical cancer when identified early.⁶



.png)